- For SME and Groups
- For Individuals
Group Health Insurance
About Cigna Healthcare
Let's Talk About Men’s Health
Entrenched notions of masculinity, risky lifestyles, a reluctance to seek medical help, and societal expectations all contribute to shorter lifespans and higher rates of male preventable illnesses. Dr. Lior Baruch, Medical Principal for Cigna Healthcare International Health, looks at what drives and deprives men’s health. Let’s talk about it.
Getting men to address their well-being is one of the great health challenges of our time. Hindered by deep-rooted notions of masculinity, only now are we taking meaningful steps to debunk stigmas associated with male mental and physical health.
Men’s health trails that of women’s across a few key metrics. Men often get sicker than women, spend more years in poor health, engage in riskier activities and die younger. The OECD’s Health At A Glance 2023 shows men live 5.4 years fewer than women, are more prone to acute and chronic heart conditions, to be diagnosed with diabetes, and to die from cancer or suicide.
But the heartbreaking fact of men’s ill-health and premature death is not the diagnosis, but the cause, which often is entirely preventable. Men engage far more in risky lifestyle behaviours, such as smoking, drinking alcohol, using drugs, eating poorly, not exercising enough, or encountering accidents.
Despite these realities, men see their doctors far less, and are more likely to report feeling in good health than women.
Maleness not a prerequisite for illness
Out of the five major threats to men – cardiovascular disease, diabetes, lung and prostate cancer and depression, two can be reasonably attributed to the inherent, male biological condition.
Heart disease is one. Women naturally have higher levels of “good cholesterol” (HDL cholesterol) than men, protecting them from heart disease. This means men must work harder earlier in life to reduce their risk of heart disease.
Diabetes is the second. While women's blood sugar creeps up more noticeably as they age, contributing to a higher prevalence in women over age 70, men show a higher prevalence of type 2 diabetes from young to middle-age, leading to more years lived in ill-health.
Social determinants, notably those long associated with masculinity, account for the remaining threats.
Take prostate cancer as an example. Raising awareness is key, since it is one of the most common cancers in men. But it grows so slow that more men die with prostate cancer than because of it. Every patient is different, and speaking with doctors about risks and the benefits of screening can lead to early detection and treatment.
However, prostate cancer is highly associated with depression and stress, as diagnosed men often anticipate treatments and potential side effects, such as immediate complications (e.g., bleeding, infection) as well as long-term sequelae (e.g., urinary incontinence, and erectile dysfunction).
Masculinity, risk taking and the social determinants of men’s health
Whether out of optimism, conformity or sheer daring, men take more risks. It’s the same when it comes to health. Men smoke, drink, use drugs and eat unhealthier, all while having fewer check-ups.
While much of these risk factors can equally be attributed to socioeconomic forces, such as wealth, education, access to health and social services, entrenched notions of masculinity, too, must be addressed.
Look at smoking, long marketed as a masculine activity. In the early days of cigarette advertising, “More Doctors Smoke Camels” was the tagline, leveraging the authoritative and masculine features of the medical profession of time. Then, the iconic Marlboro Man led campaigns for almost 40 years, embodying all the tough, rugged, daring and independent notions of masculinity.
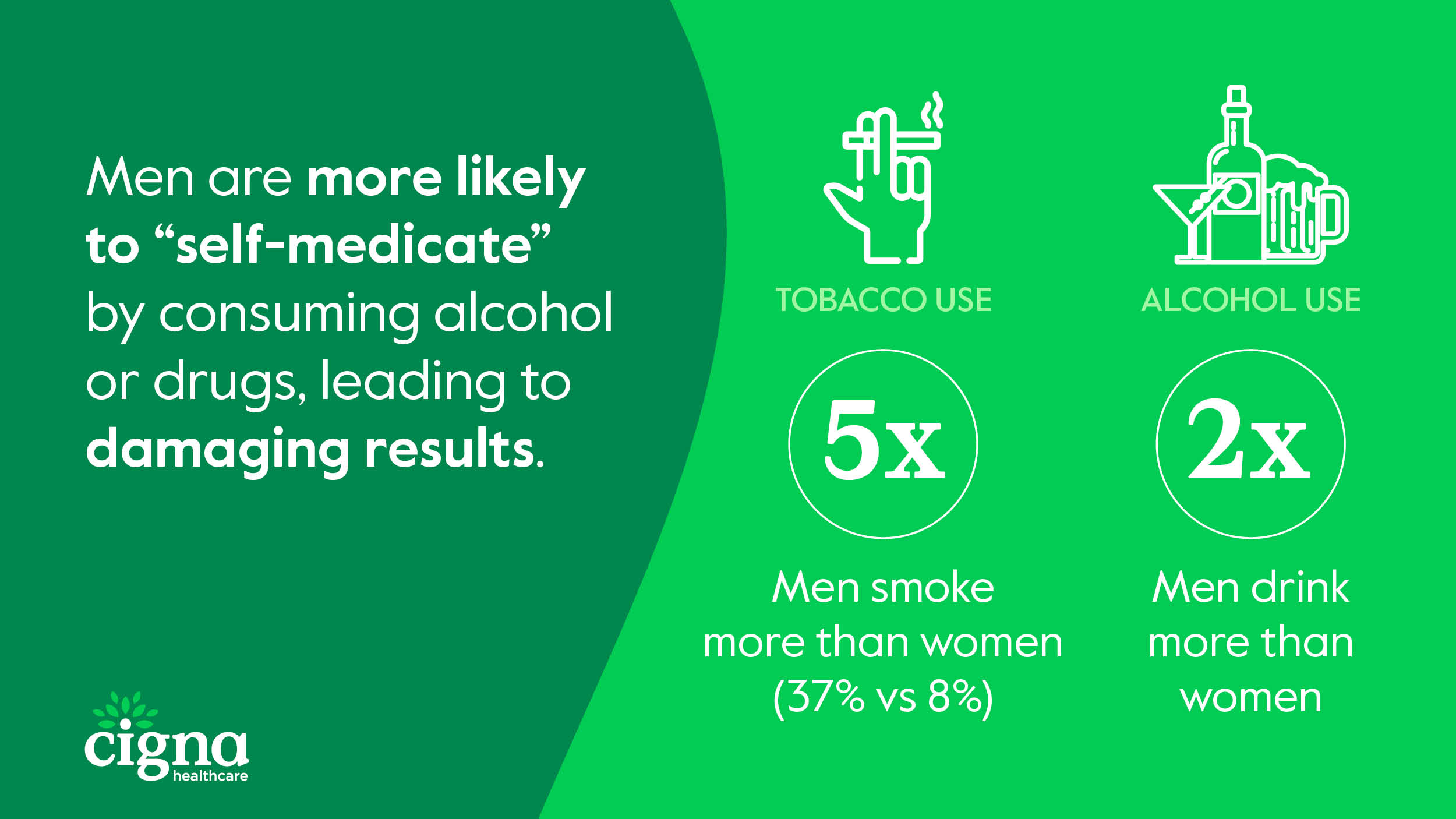
Sadly today, the consequences of that protracted campaign are playing out. Around 37% of men use tobacco, compared with 8% of women, causing 1 out of every 5 male deaths globally.
The same can be said for alcohol use. For decades, advertisers leveraged similarly masculine attributes (tough, daring and independent) to target male consumers. Today, men drink about twice that of women.
Physical health consequences of alcohol and drugs abound, from high blood pressure and heart disease to stroke, liver disease, and digestive problems. But substance abuse also intervenes severely with male mental well-being.
Emotional suppression is one especially concerning link. Rather than expressing emotions through less destructive channels, men are more likely to “self-medicate” by consuming alcohol or drugs, leading to much more severe and devastating results.
Suicide, mental health and the new frontline in men’s well-being
Every year, millions of people must say goodbye to a partner, brother, father, son, uncle, cousin or friend too soon. While incidents are generally on the decline, male suicide rates consistently double that of females, across every international measure.
Suicide can be caused by any number of reasons. Often it is triggered by a crisis or stress, whether financial, personal, health or pain related, or by conflict, disaster, violence, abuse, discrimination, loss or a sense of isolation. Mental health conditions exacerbate and amplify these.
Biologically, being male comes with a few unique vulnerabilities linked with the development of suicidal thoughts. On one hand, researchers have found the immune system, sex hormones and puberty all heighten suicide vulnerability, especially in adolescents. While male impulsivity has been directly linked to the development of the prefrontal cortex — the brain’s control centre – which forms later in males than females.
Men’s mental health, however, is extremely susceptible to external, social factors due in large part to their tendency towards emotional suppression and aversion to seeking help.
It's not to say that they have different conditions, or they don't face the same challenges as women. But there remains severe stigma around men’s mental health.
Entrenched, outdated notions of masculinity lead many men to suppress or avoid expressing emotion for fear of appearing weak or being ridiculed. For young boys, such barriers to expressing emotion can lead to anxiety and other mental health issues.

Men need to see and talk to their doctors more
As the father of two young boys, instilling healthy habits and dispelling outdated myths around masculinity are among my greatest concerns. We know, from years of research that certain, outdated masculine attributes and behaviours can increase risk-taking, causing earlier onset of ill-health, triggering mental health issues and preventing them from seeking professional help.
But it isn’t just the younger men that encounter these challenges. Males of almost all ages are considered higher risk when it comes to mental and physical ill-health and premature death.
For men in their 30s and 40s who have families and dependents, for example, their unwillingness to see their GP regularly or pick-up on conditions early is perhaps their greatest flaw.

The fact is: if a man is not experiencing a serious or acute health concern, he simply won’t have a regular health or wellness check-up. Even when sick, it is likely he will delay care. Again, all stemming from masculine beliefs which reinforce self-reliance over seeking support. Family dynamics often reinforce this.
Considering men are more likely to be diagnosed with and die at higher rates from cancers that can be prevented, it is especially worrying that healthcare avoidance (driven by outdated beliefs) may be undermining life-saving access to screening.
Harder still, male participation in life-saving screenings worsens as the prevalence of mental ill-health rises. For those invested in improving outcomes for men, the question is: How do we create tailored health and well-being programs, and awareness campaigns, that overcome notions of self-reliance, masculinity and doctor avoidance?
Addressing men’s health and masculinity through a new lens
Some detrimental notions of masculinity will continue to hinder men’s health for some time. But doctors, healthcare providers, parents and communities all have the power to change this through Awareness, Communication and Education.
For doctors, delivering optimal men’s healthcare first requires trust – early and throughout a man’s life. Whether that be by adopting more "male-oriented" approaches in your clinic, utilising messaging that emphasizes strength over deficit, dispelling myths around weakness or addressing family, finance and work-related issues in the same breath as a diagnosis.
For parents, communities and men everywhere, improving Awareness, Communication and Education relies on a few key well-being principles.
- It starts at home. Parents and siblings must work to help their young male family members to speak openly about their health and well-being as early as possible. Expressing emotions is just as difficult as learning a new language, but with practice, we get there.
- Don’t wait. Schedule regular check-ups with your primary care provider. Ask questions to help you make healthier decisions and identify, treat and prevent underlying issues. There are no wrong questions upon a consultation – speak freely.
- Embrace routine screenings. They detect diseases early and make treatment more effective. Include screenings for cholesterol, blood pressure, diabetes, and other risk-related conditions, which vary by every patient and lifestyle. Paediatricians play a key role in training children to accept screening as a normal part of life from early on.
- Adopt healthier habits. Eat better and incorporate regular exercise into your routine. Limit alcohol intake, and always consider quitting smoking.
- Be brave. Recognize when you aren’t doing ok, or when you’re not feeling yourself. Asking for help, or just accepting it, changes your life. Addressing mental health conditions like depression, anxiety, and substance abuse start with breaking the stigma around seeking help (clinical or personal) for mental health concerns.
- Break the silence and talk about men's health. Talk about it and connect with other men in your life, family and colleagues. No amount of toughing it out, manliness or ruggedness is worth risking your health. Feeling heard, and being surrounded by people that are truly interested in you – as a person – can change your life perception.
These are lessons we should be teaching our sons, and talking about with our partners, brothers, fathers, uncles, cousins and friends.
Get a Quote Today
Let our consultants prepare and arrange a customised group health insurance plan that best meets your needs.
Contact Us
Popular Links
Resources
Connect with us
© 2024 Cigna Healthcare. All rights reserved.
Cigna Europe Insurance Company S.A.-N.V. Singapore Branch (Registration Number: T10FC0145E), is a foreign branch of Cigna Europe Insurance Company S.A.-N.V., registered in Belgium with limited liability, with its registered office at 152 Beach Road, #33-05/06 The Gateway East, Singapore 189721.
The Cigna Healthcare name, logo, and other Cigna Healthcare marks are owned by The Cigna Group Intellectual Property, Inc. licensed for use by Cigna Corporation and its operating subsidiaries. All products and services are provided by or through such operating subsidiaries, and not by Cigna Corporation. Such operating subsidiaries include Cigna Europe Insurance Company S.A.-N.V. Singapore Branch.

